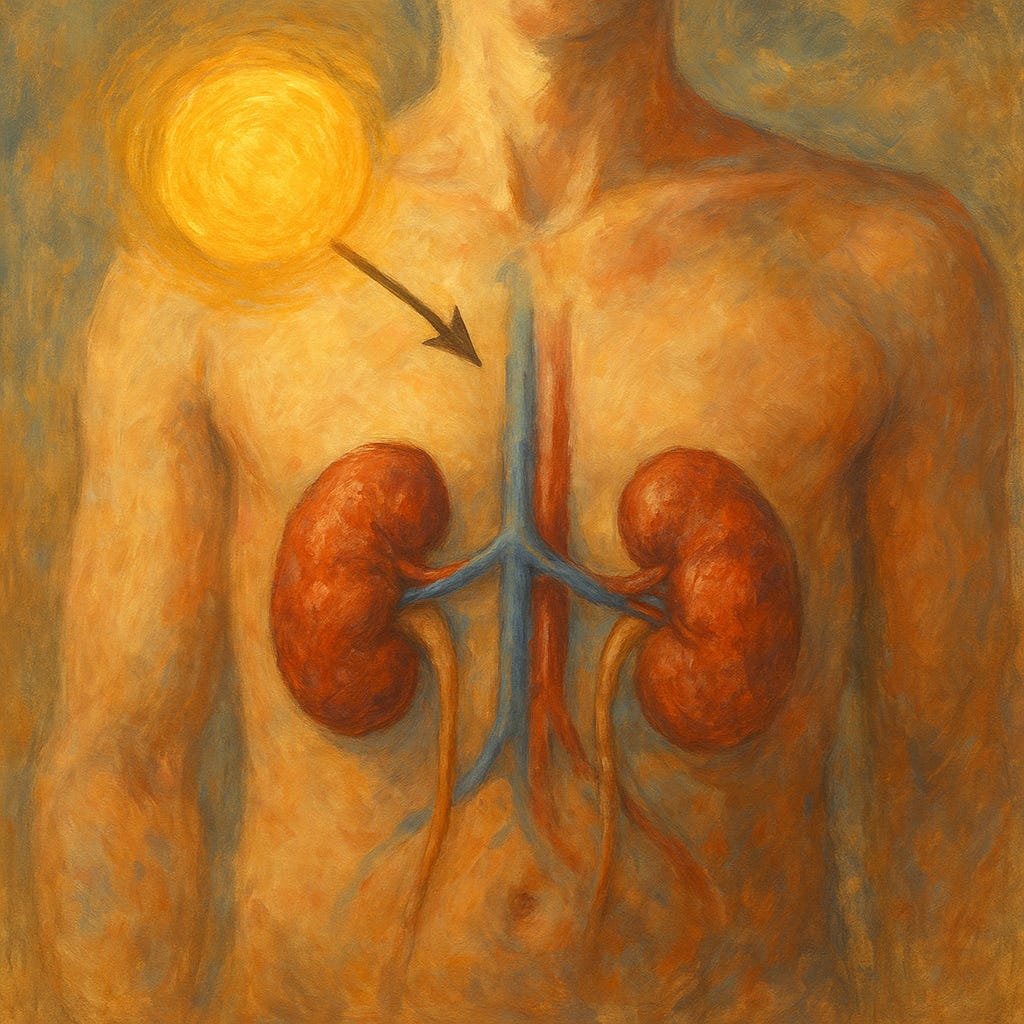
Vitamin D Strategies in Chronic Kidney Disease Patients Need Personalization
New findings show that routine supplementation and testing may not benefit all CKD patients equally, highlighting the need for an individualized approach.
Topline:
Recent research presented at the National Kidney Foundation 2025 Meetings emphasizes that while vitamin D levels are often dysregulated in CKD patients, routine supplementation and testing offer uncertain benefits and should be personalized based on each patient's risk factors and clinical context.
Study Details:
At the NKF 2025 Spring Clinical Me…
Keep reading with a 7-day free trial
Subscribe to Just Healthcare to keep reading this post and get 7 days of free access to the full post archives.