Understanding Muscle Changes During GLP-1 Treatment
What current human and imaging data show about lean mass, muscle quality, and physical function during GLP-1 treatment.
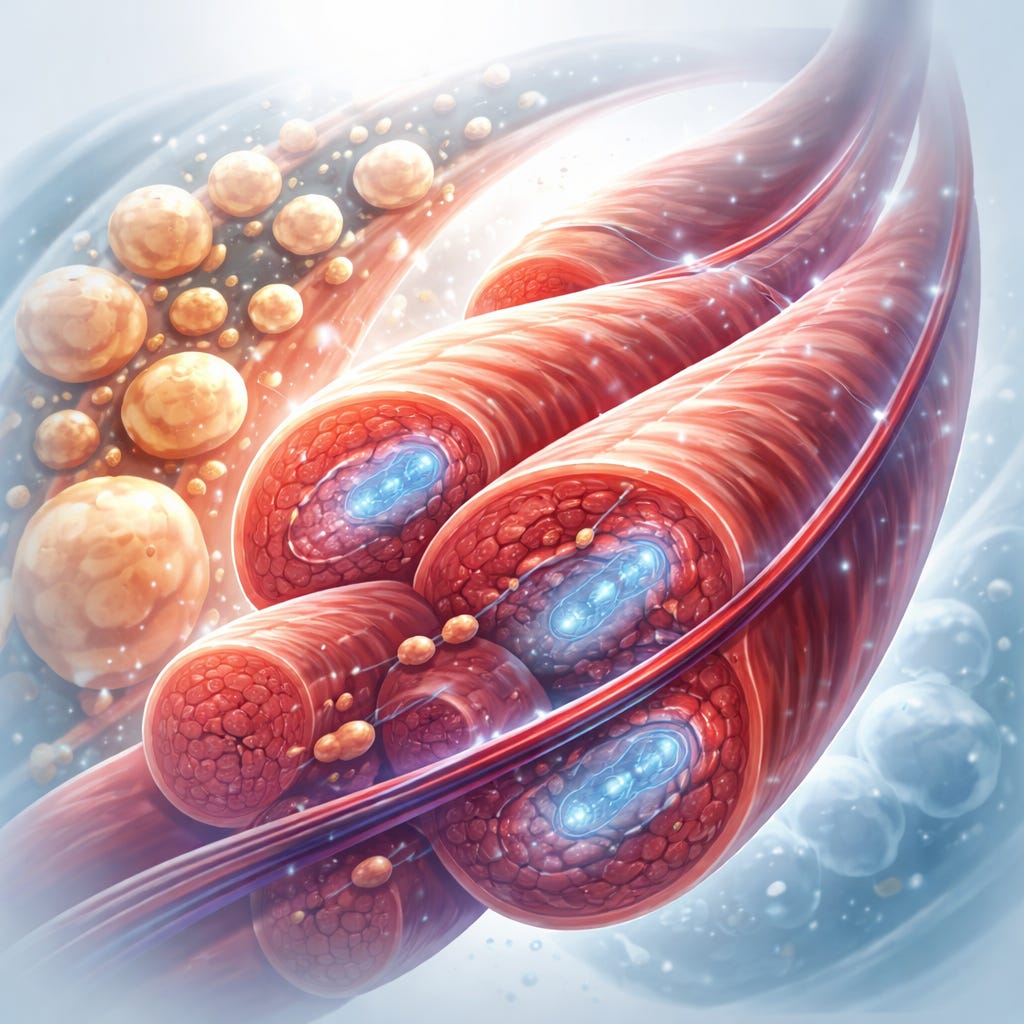
Current evidence suggests GLP-1 receptor agonists lead to modest reductions in absolute muscle mass that track with overall weight loss, while muscle quality, metabolic efficiency, and functional performance are largely preserved or improved.
Study Details
GLP-1 receptor agonists have reshaped treatment for obesity and type 2 diabetes by delivering sustained weight loss and cardiometabolic benefits. As use expands, clinicians and patients have raised concerns about unintended muscle loss, particularly in older adults and people with long-standing diabetes who already face elevated risk of sarcopenia.
Recent analyses summarized by endocrinology experts reviewed randomized trials, MRI-based substudies, and mechanistic research evaluating how GLP-1 therapies affect skeletal muscle quantity and quality during weight loss.
Methodology
Researchers synthesized data from randomized clinical trials and meta-analyses assessing body composition changes during GLP-1 therapy. Advanced imaging, particularly MRI, was used to distinguish absolute muscle volume from lean body mass and to quantify intramuscular fat infiltration. Selected trials, including detailed imaging sub analyses from weight-loss studies, also examined muscle composition, insulin sensitivity, and metabolic signaling pathways.
Key Findings
Reductions in lean body mass during GLP-1 therapy generally account for about 12 to 40 percent of total weight loss, often clustering at the lower end of this range.
Absolute muscle mass declines appear proportional to total weight reduction and do not exceed expected physiologic responses to weight loss.
When expressed as a percentage of body weight, lean mass is often unchanged or increased, suggesting fat loss predominates.
MRI studies show consistent reductions in intramuscular fat, indicating improved muscle quality despite modest volume loss.
Functional measures such as strength and physical performance appear largely preserved in available clinical data.
Implications for Practice
For patients, these findings suggest that muscle changes seen with GLP-1 therapy are not equivalent to pathologic muscle wasting. Improvements in muscle composition, insulin sensitivity, and mitochondrial efficiency may help maintain strength and function even as body weight declines.
For clinicians, the data support reframing lean mass loss during GLP-1 treatment as a physiologic adaptation to weight reduction rather than a harmful adverse effect. Emphasis should remain on resistance and weight-bearing exercise, along with adequate dietary protein, to further protect muscle health. This approach appears especially important for older adults and those with diabetes or chronic kidney disease.