Restoring the Brain’s Sugar Shield Could Protect Against Alzheimer’s and Aging Damage
New research shows repairing the blood-brain barrier may reverse cognitive decline in preclinical models
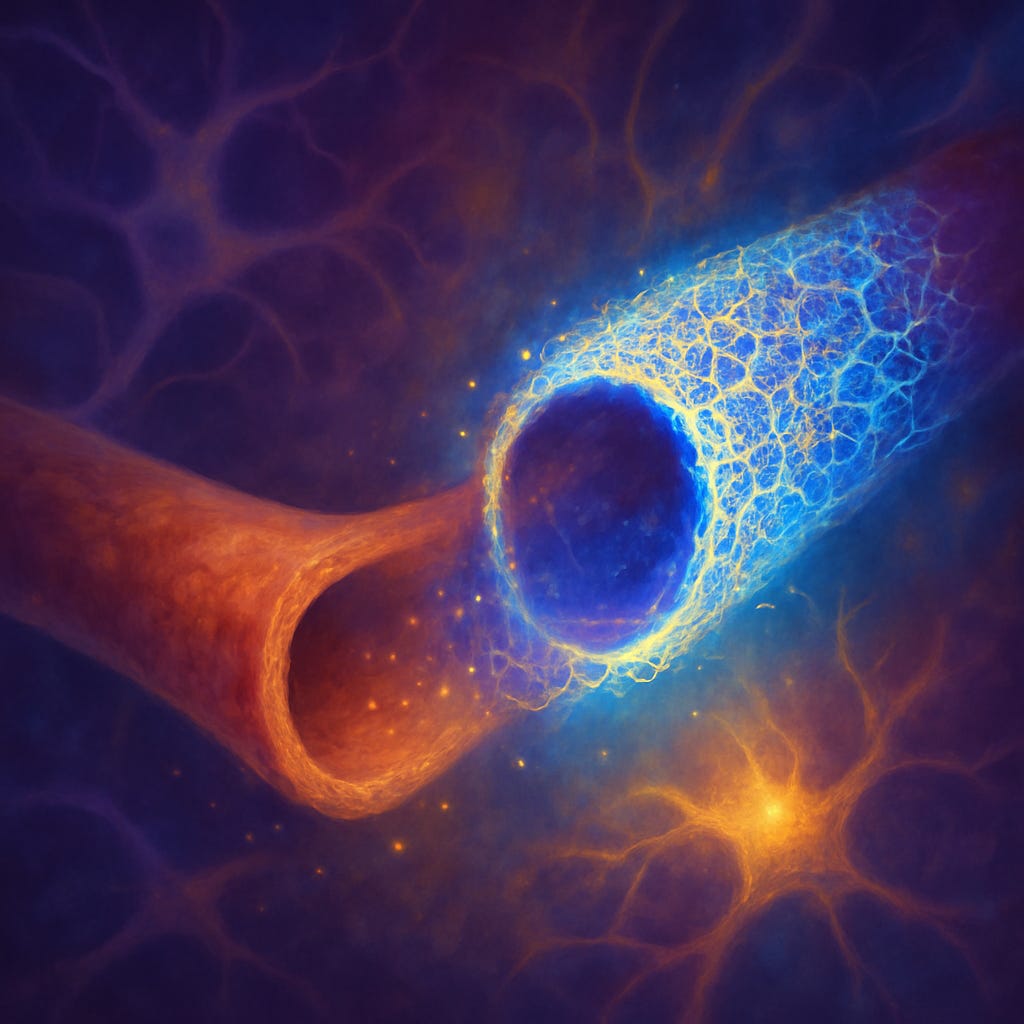
Scientists have identified age-related damage to the brain’s blood-brain barrier (BBB) caused by the breakdown of a protective sugar-rich layer called the glycocalyx.
In mice, restoring this “sugar shield” improved barrier function, reduced inflammation, and enhanced cognitive performance, offering a promising new approach to treating Alzheimer’s, Parki…
Keep reading with a 7-day free trial
Subscribe to Just Healthcare to keep reading this post and get 7 days of free access to the full post archives.