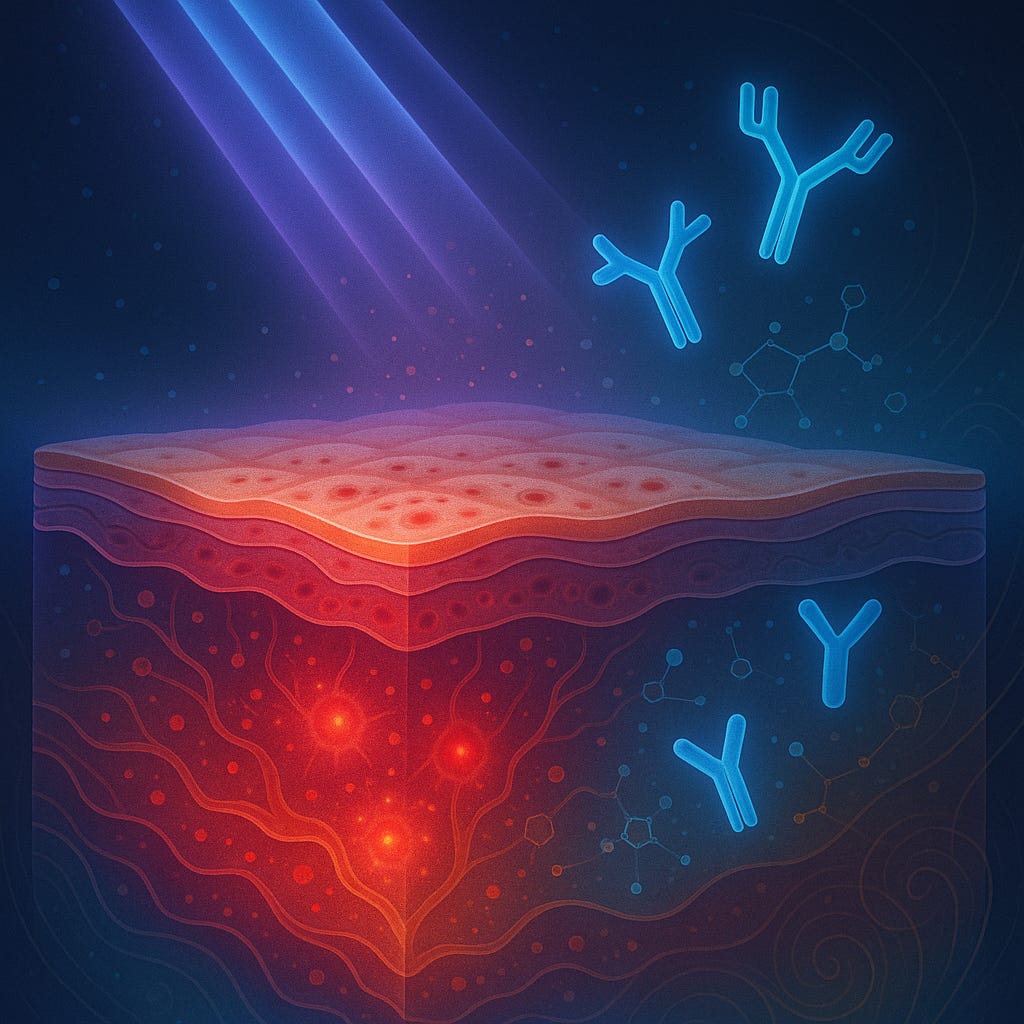
Monoclonal Antibodies and JAK Inhibitors Show Real Progress for Photosensitive Skin Disorders
Emerging targeted therapies may improve symptoms and quality of life for people living with chronic sunlight-triggered skin conditions.
A new systematic review suggests that monoclonal antibodies and JAK inhibitors may offer meaningful symptom relief and improved sunlight tolerance for several photosensitive skin disorders, including chronic actinic dermatitis, actinic prurigo, solar urticaria, photoaggravated eczema, photoaggravated psoriasis, and polymorphic light eruption. Although t…
Keep reading with a 7-day free trial
Subscribe to Just Healthcare to keep reading this post and get 7 days of free access to the full post archives.