Immune System Signals May Slow Fat Burning
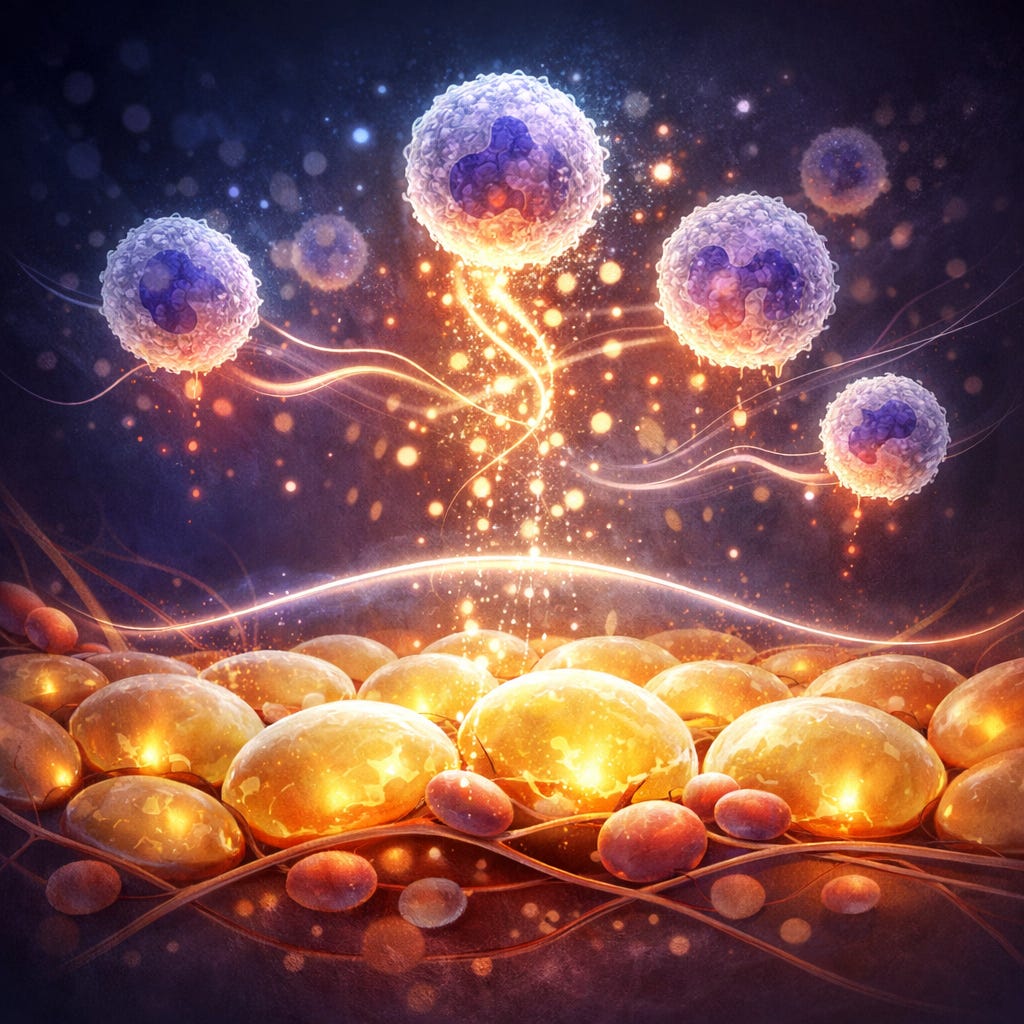
New research suggests immune cells actively regulate how quickly the body releases stored fat during stress, with implications for obesity and metabolic disease.
A Nature study finds that neutrophils release inflammatory signals that slow fat breakdown during cold exposure or fasting, revealing an immune-driven brake on energy expenditure that may contribute to obesity and insulin resistance.
Study Details
The immune system is best known for fighting infections, but new research suggests it also plays a role in re…
Keep reading with a 7-day free trial
Subscribe to Just Healthcare to keep reading this post and get 7 days of free access to the full post archives.