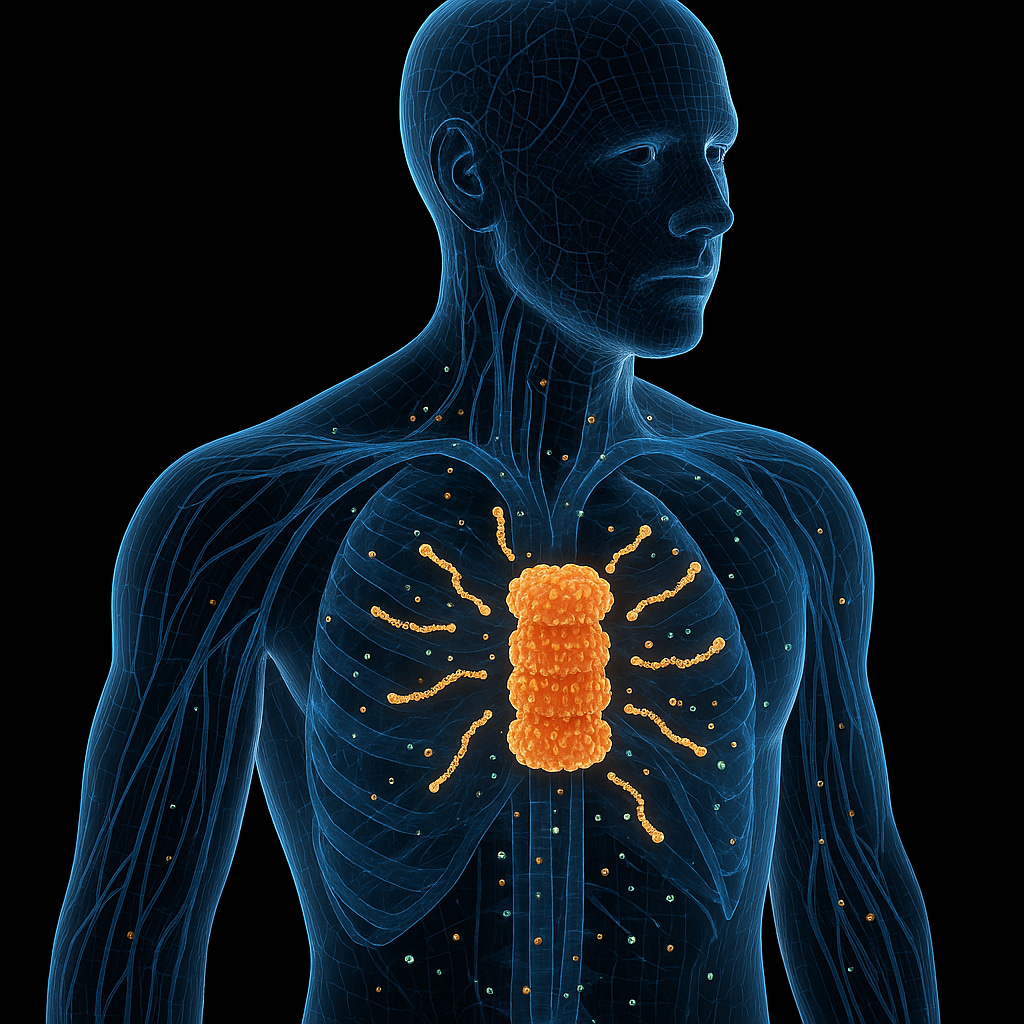
Humans Have a Hidden Immune Weapon Against Bacterial Infections
New research reveals proteasomes do more than recycle proteins—they generate bacteria-killing peptides
Keep reading with a 7-day free trial
Subscribe to Just Healthcare to keep reading this post and get 7 days of free access to the full post archives.