Extracorporeal Life Support Saves Lives in Severe Accidental Hypothermia
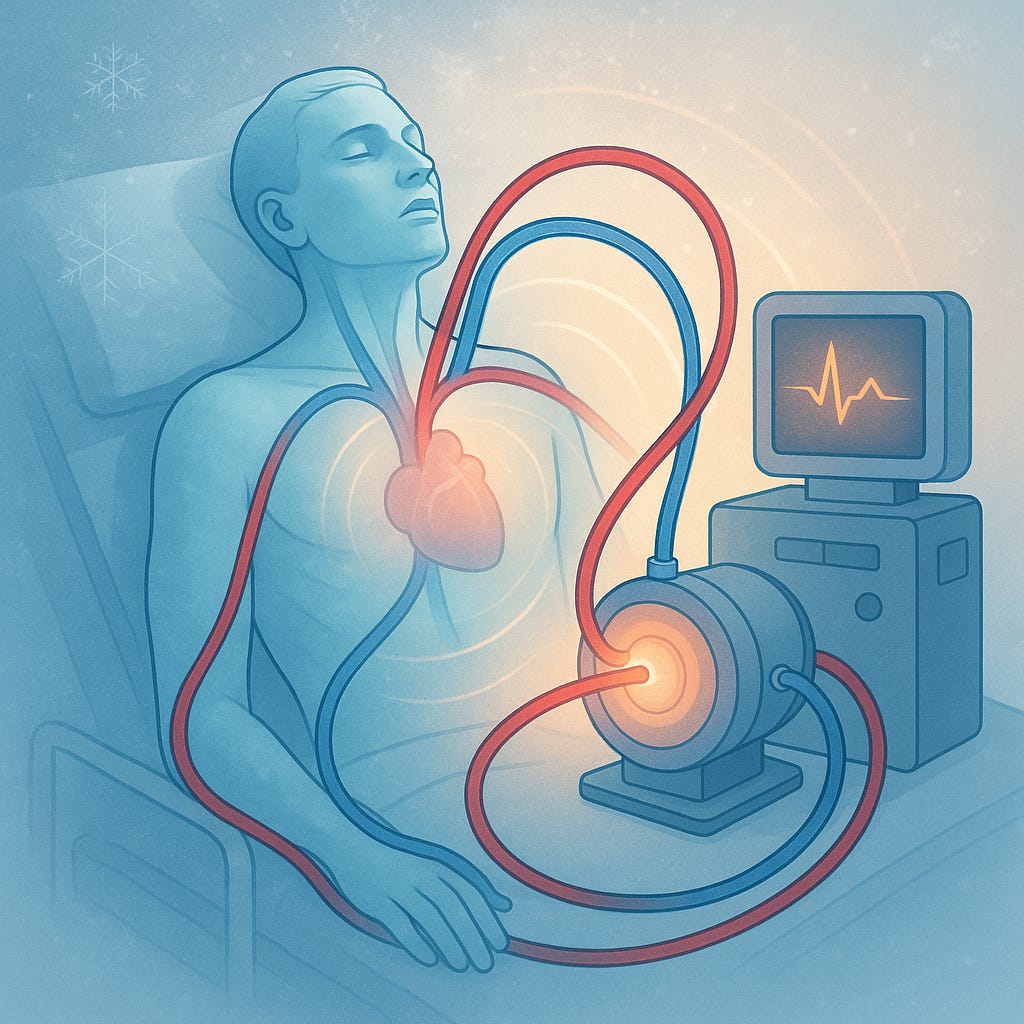
New evidence highlights how ECMO-based rewarming can restore heart function and neurological recovery in deep hypothermia cases.
Topline:
For patients with accidental hypothermia and cardiac arrest, extracorporeal life support (ECLS), primarily using ECMO, significantly improves survival and neurological outcomes compared with conventional rewarming methods.
Study Details:
Accidental hypothermia, defined as an unintentional core temperature below 35 °C (95 °F), can occur in any envi…
Keep reading with a 7-day free trial
Subscribe to Just Healthcare to keep reading this post and get 7 days of free access to the full post archives.