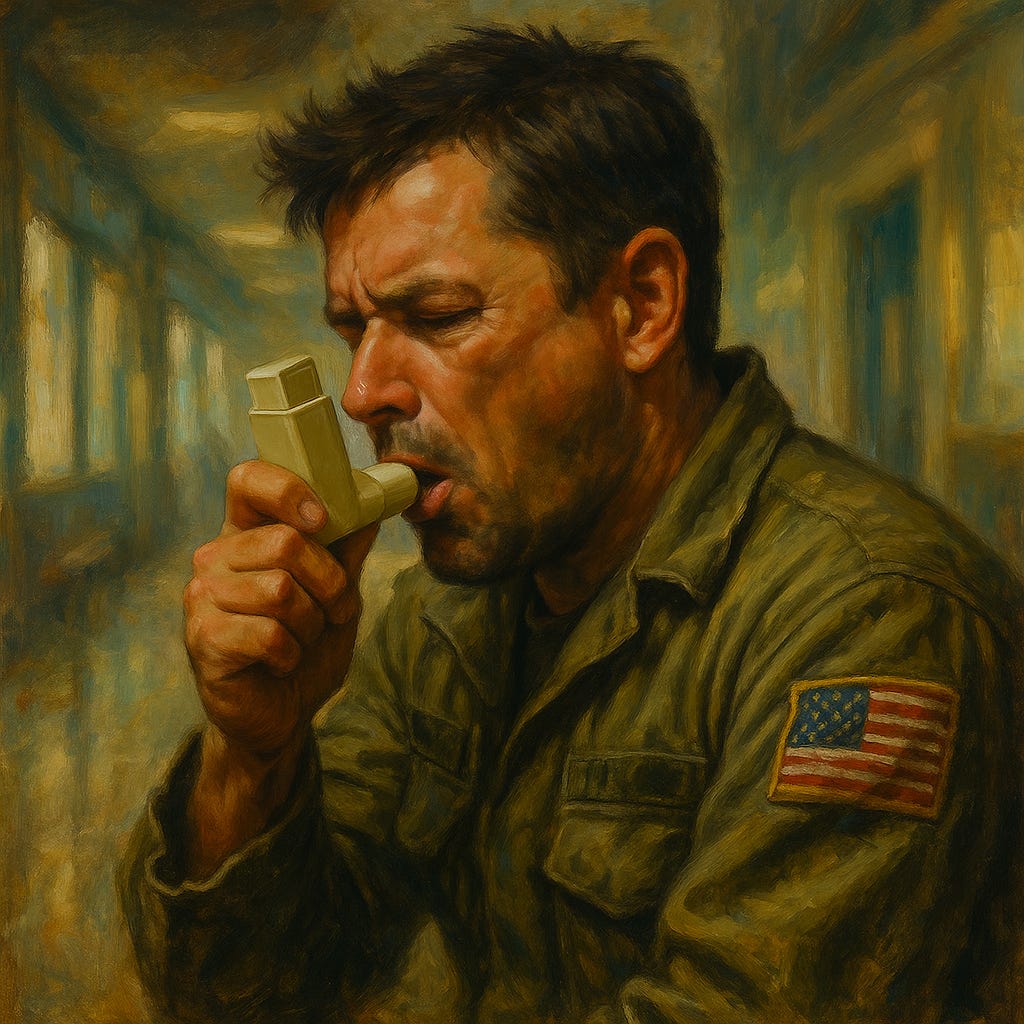
Environmentally Friendly Asthma Inhalers May Increase Hospitalizations
Large VA study links dry powder inhalers to higher emergency visits in older asthma patients
A massive observational study in the US Veterans Health Administration found that switching asthma patients from metered-dose inhalers (MDIs) to dry powder inhalers (DPIs) led to increased hospitalizations and emergency department visits, raising questions about the trade-offs between environmental benefits and patient outcomes.
Study Details
In 2021, the…
Keep reading with a 7-day free trial
Subscribe to Just Healthcare to keep reading this post and get 7 days of free access to the full post archives.